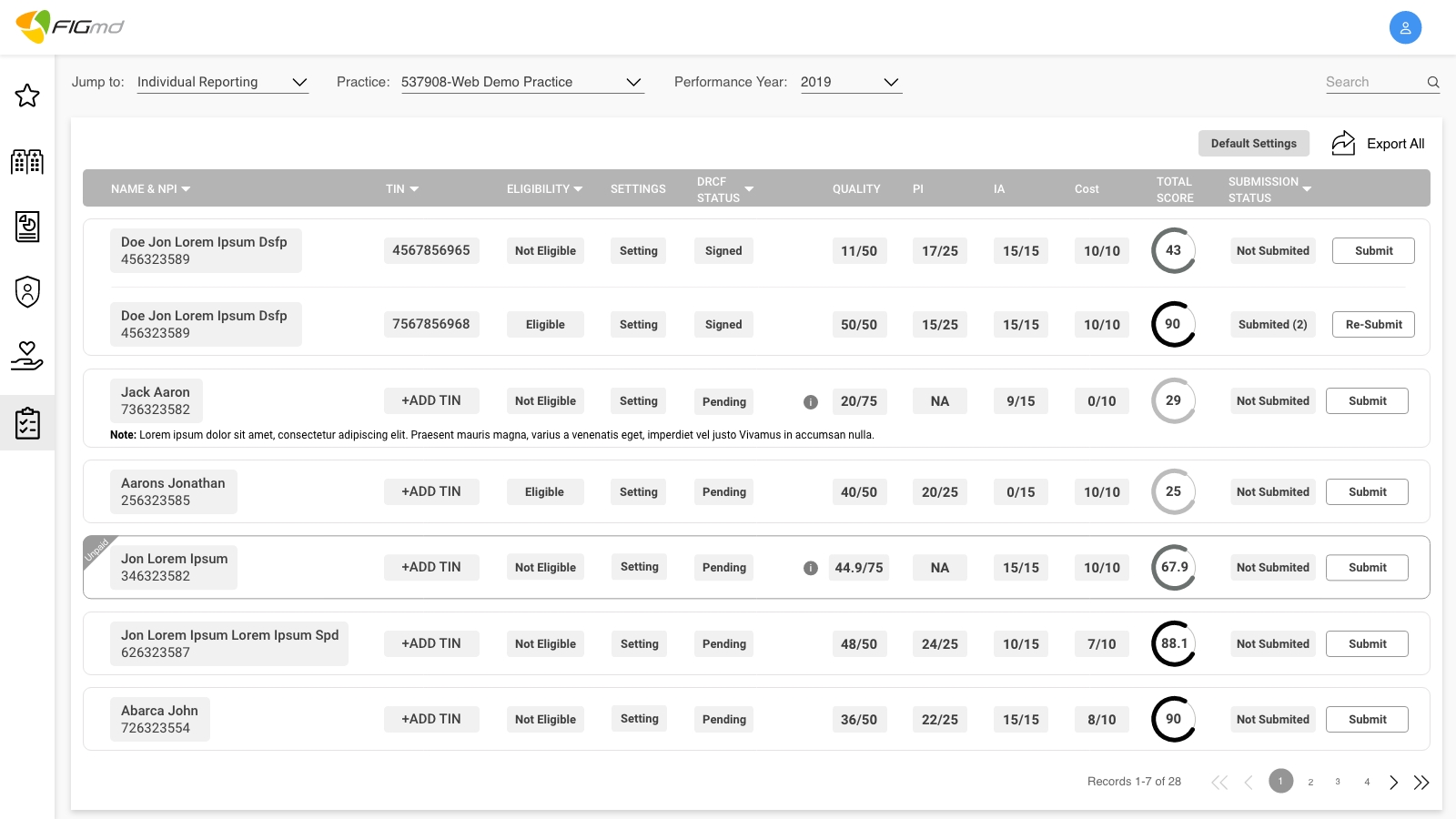
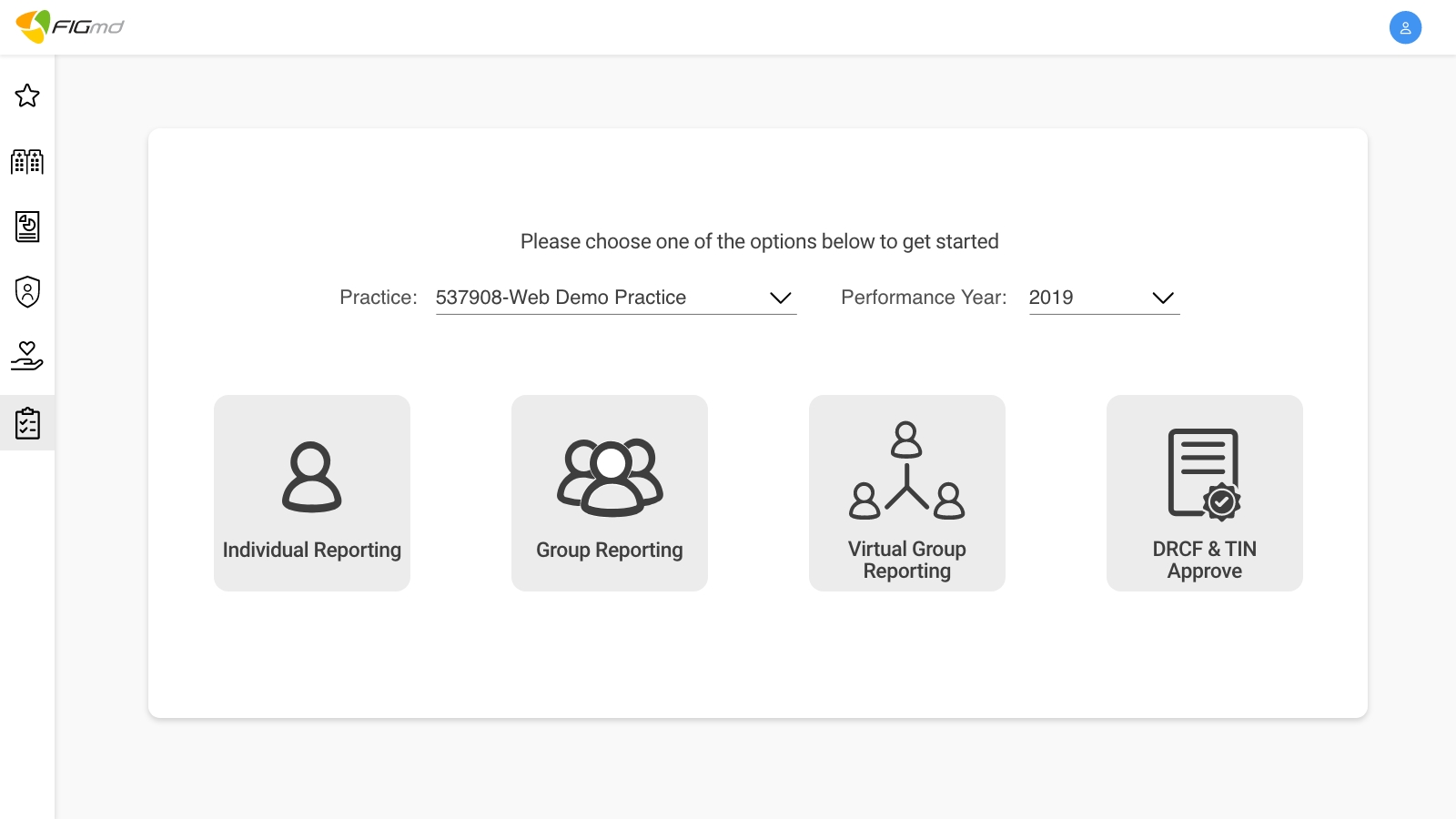
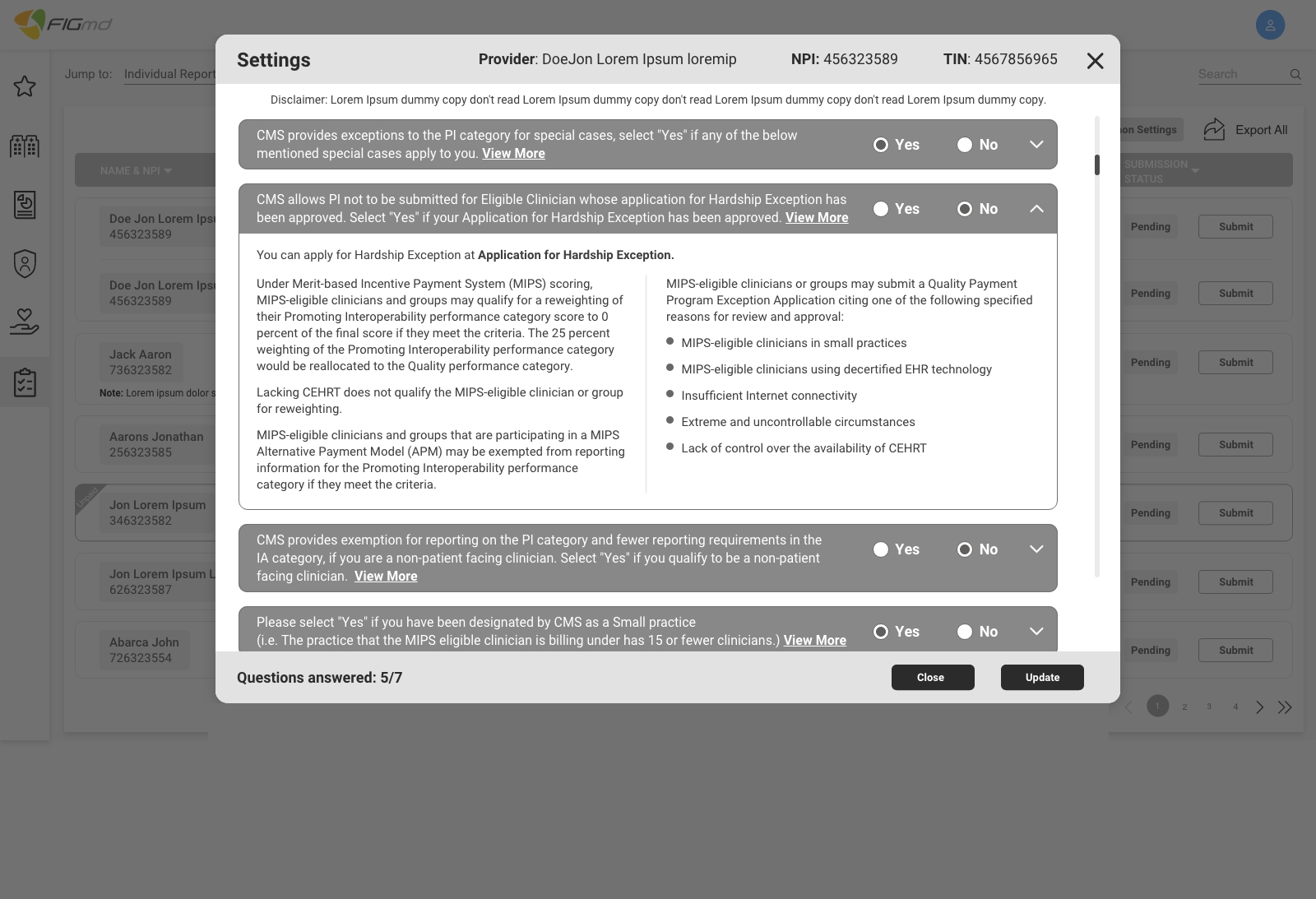
MIPS: Merit-based Insensitive Payment System
The establishment of MIPS provides an opportunity to revise, rework and improve the existing Medicare programs focused on quality, costs, and use of electronic health records to improve their relevance to real-world medical practice and reduce administrative burdens for physicians.
Medicare's legacy quality reporting programs were consolidated and streamlined into the Merit-based Incentive Payment System, referred to as "MIPS." This consolidation reduced the aggregate level of financial penalties physicians otherwise faced, and it also provides a greater potential for bonus payments.













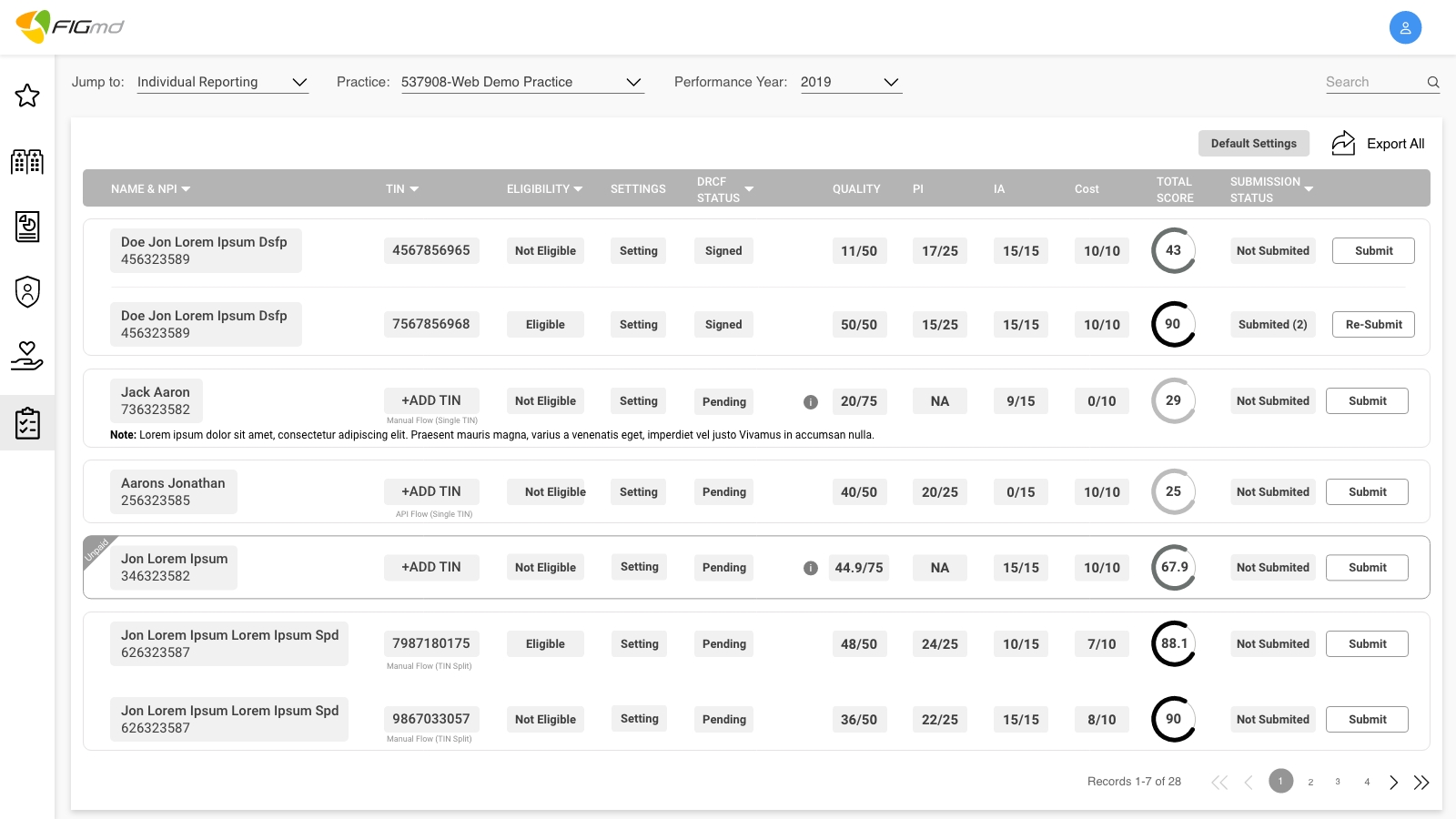
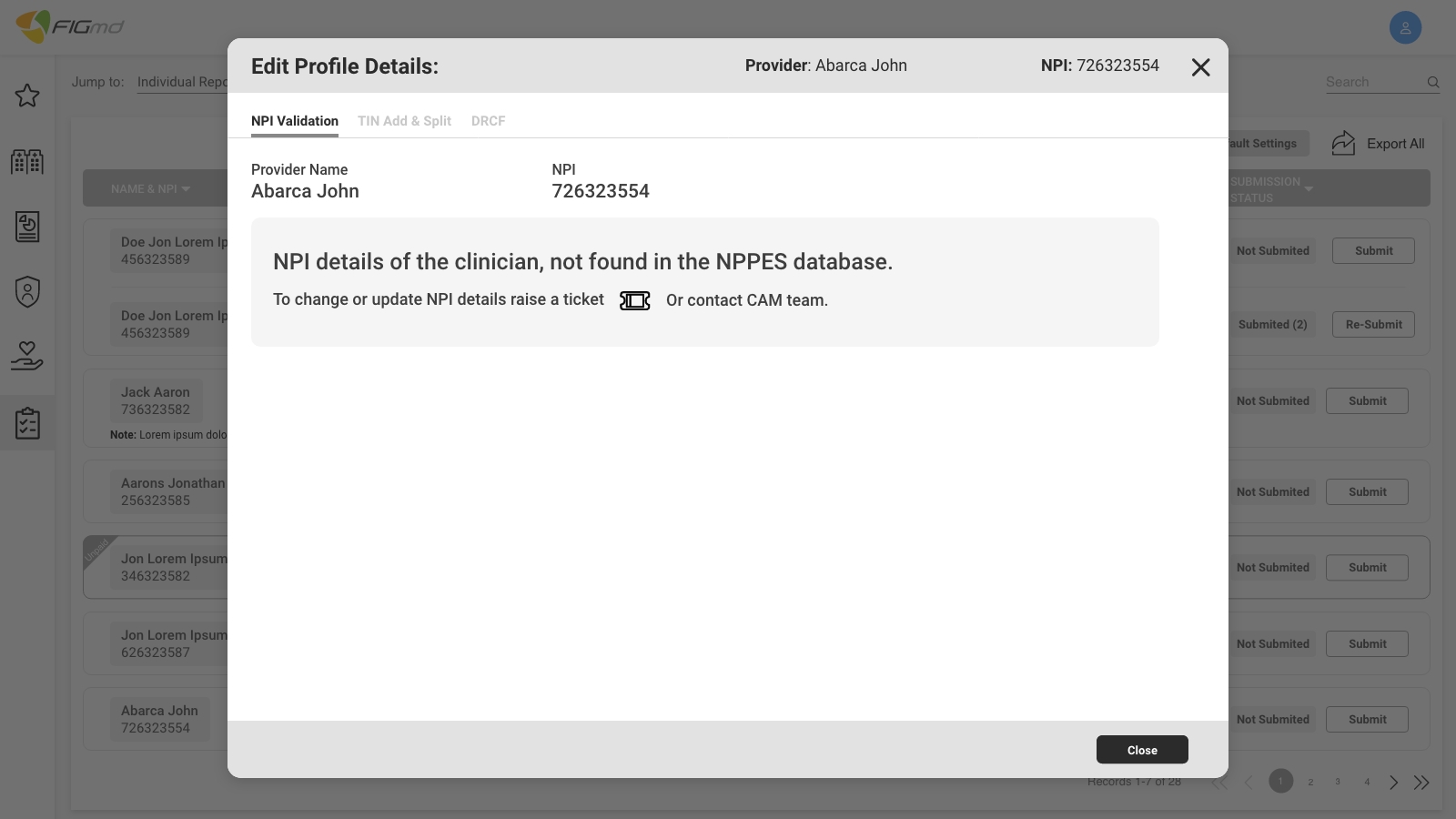
.jpg)
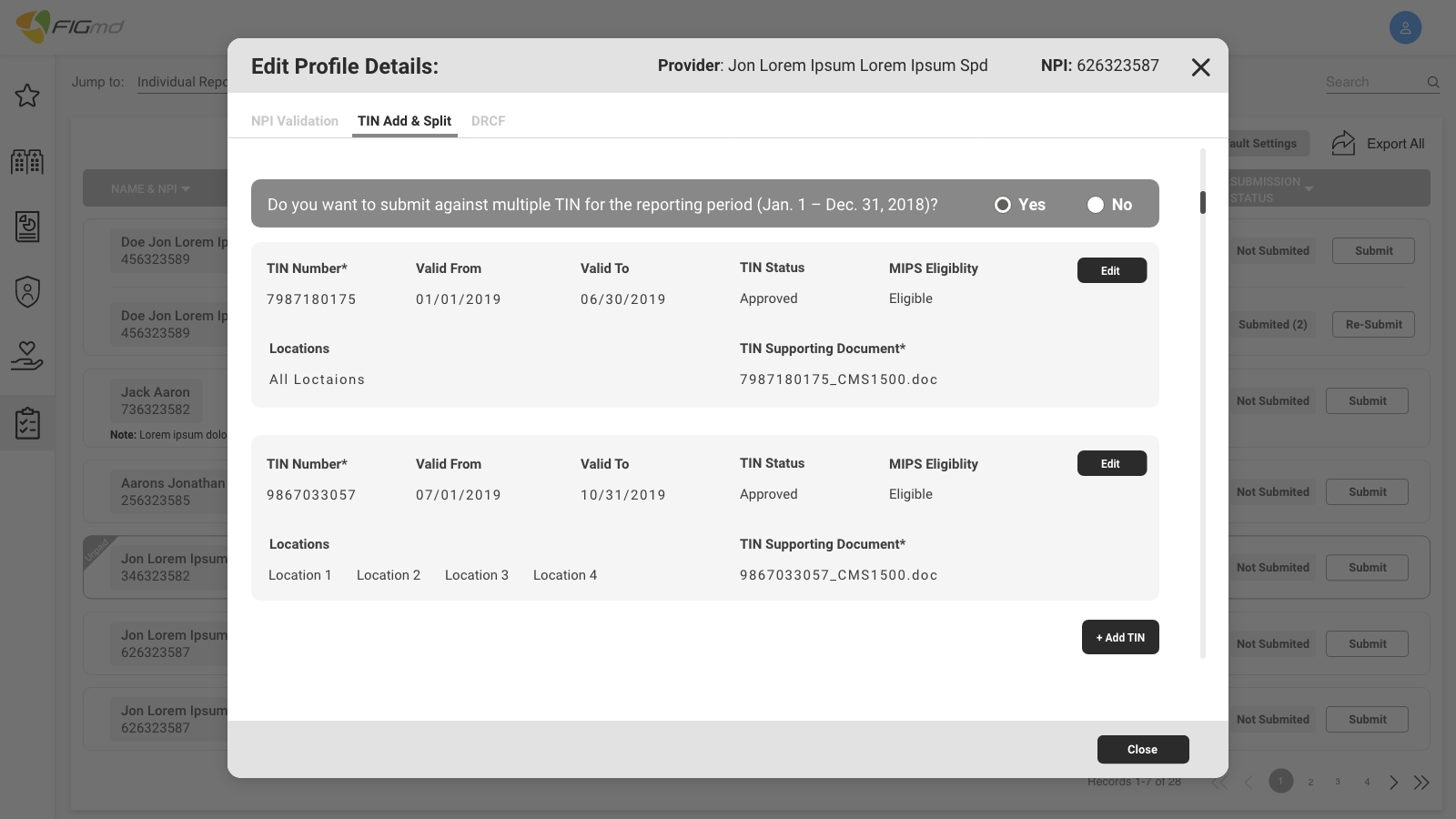
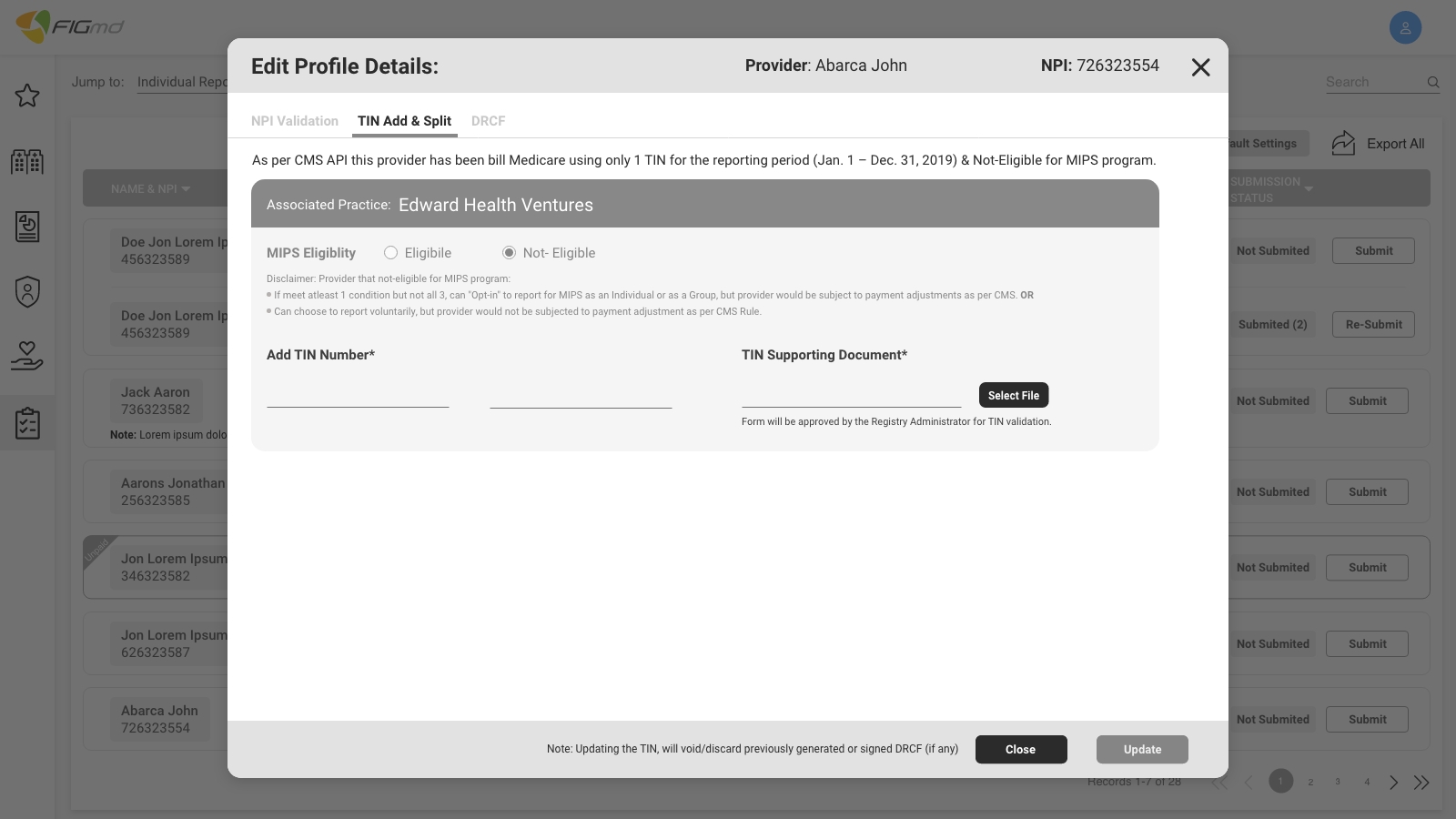
 – 1.jpg)
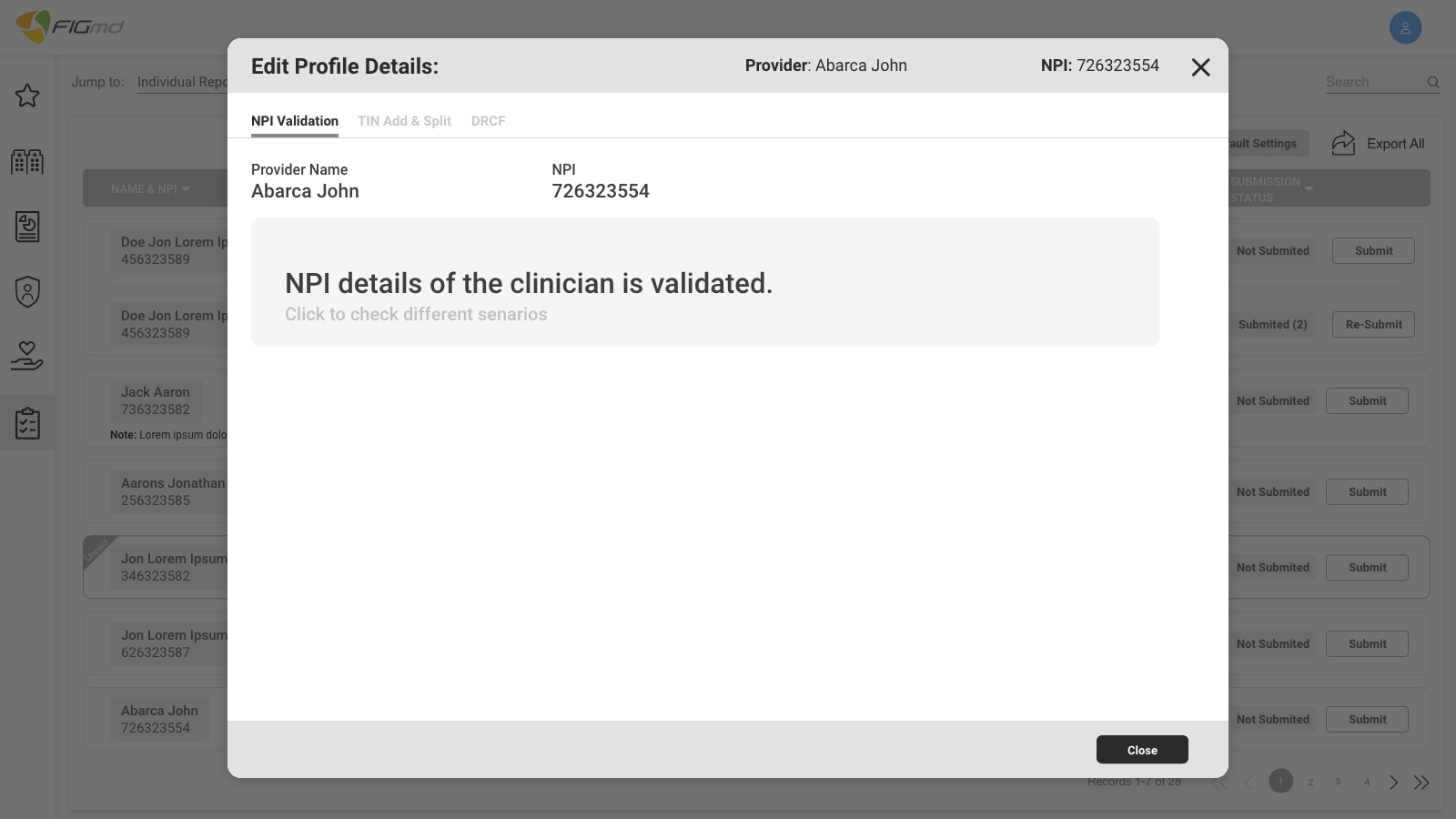
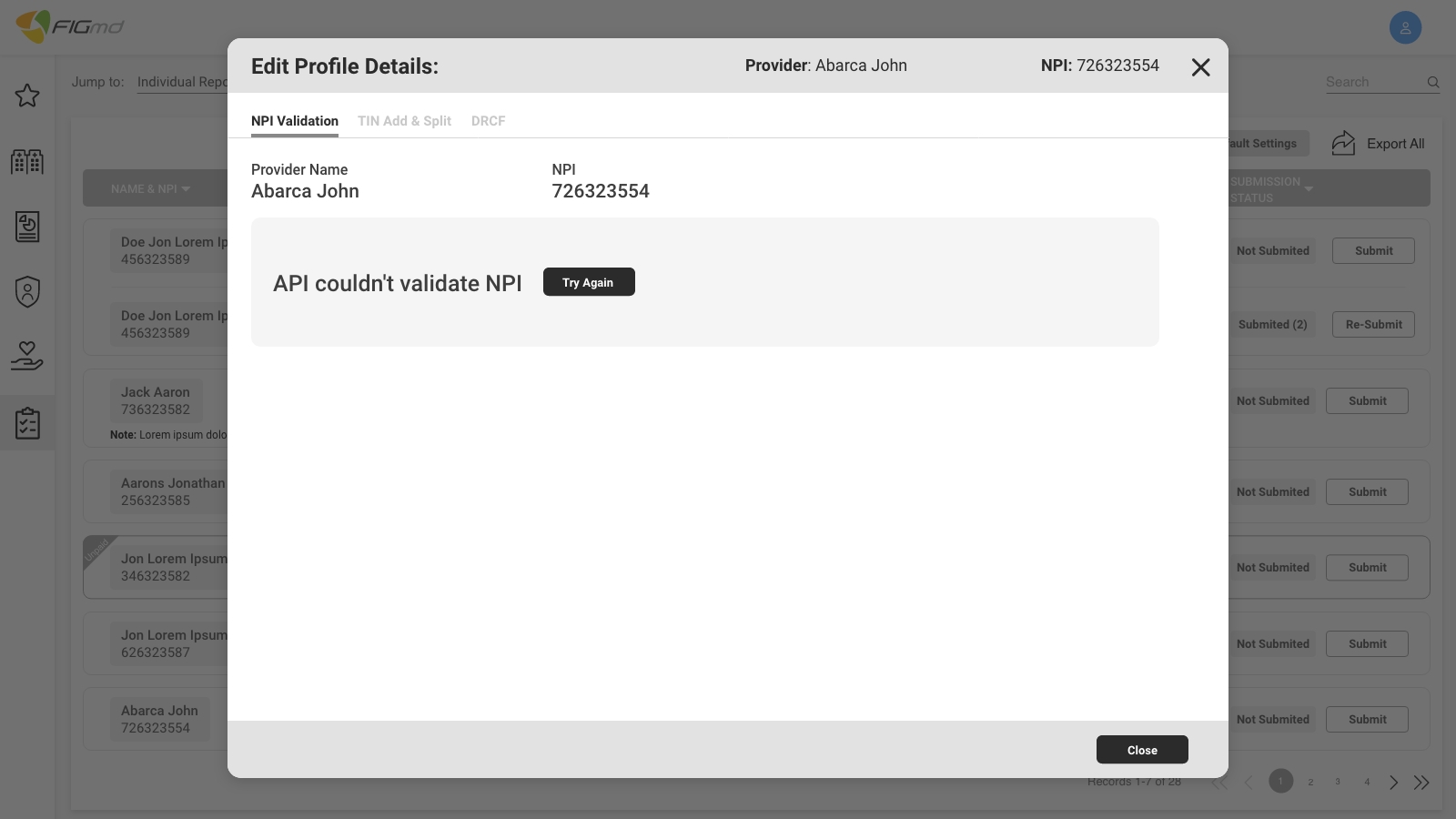
.jpg)
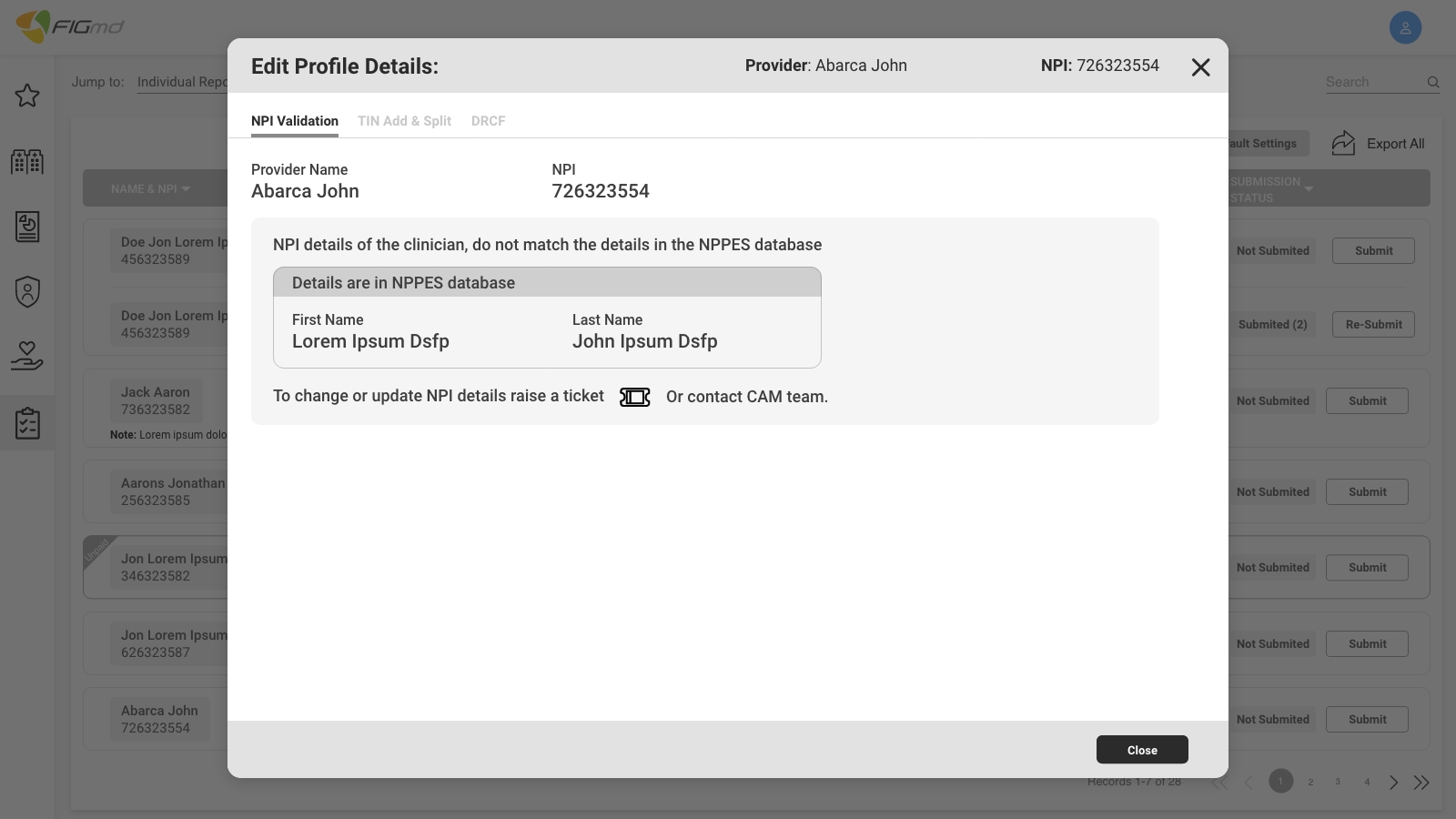
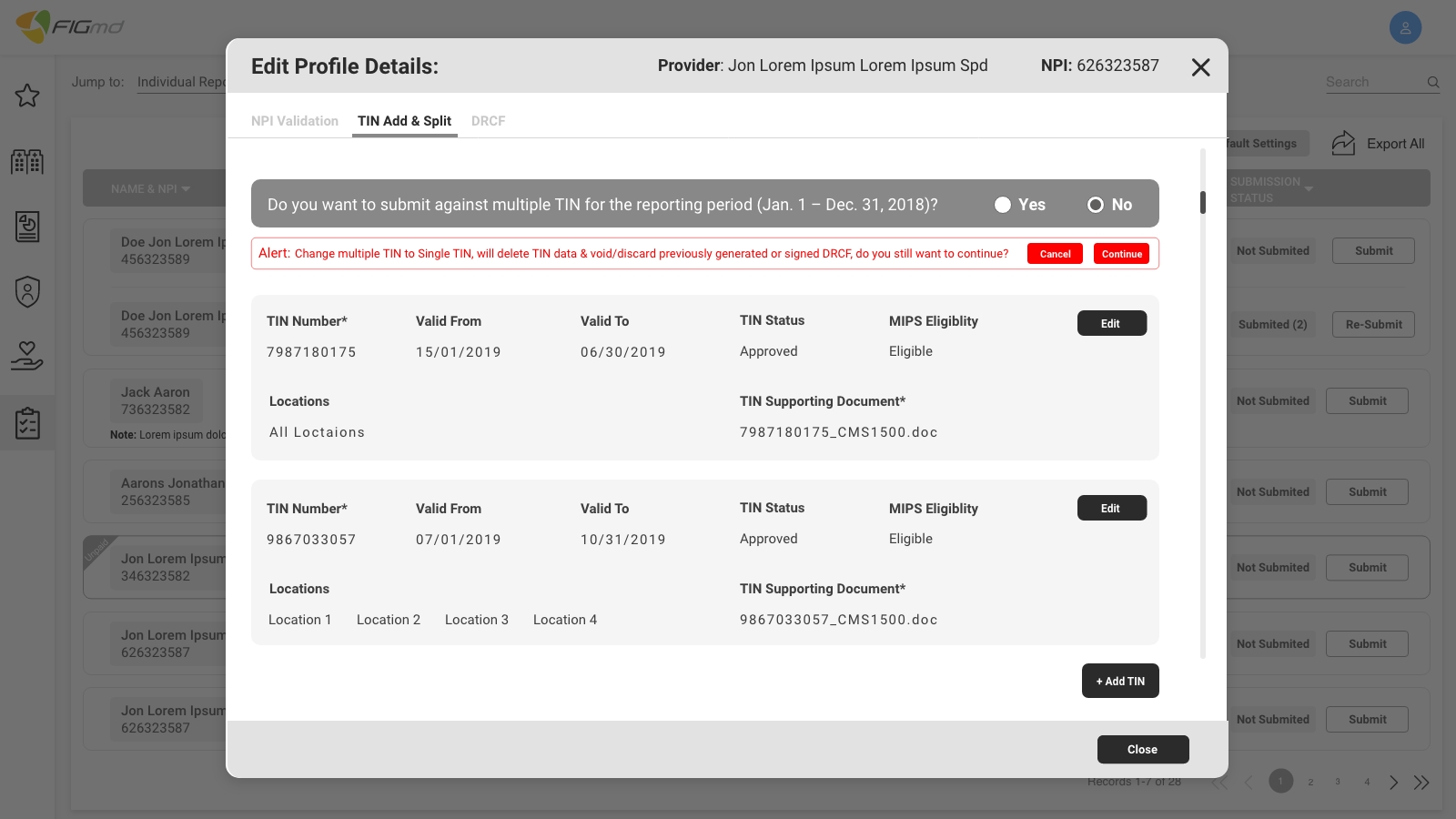
 - 1.jpg)